Food
Publisher Platform: FDA is on the hunt for Cyclospora
What is Cyclospora?
Cyclospora is a parasite consisting of one cell, too small to see without a microscope. The organism was previously thought to be a blue-green algae or a large form of it Cryptosporidium. Cyclospora cayetanensis is the only species of this organism found in humans.
Cyclosporiasis is an intestinal disease caused by the parasite Cyclospora cayetanensiswhich is transmissible by ingestion of fecally contaminated food or water.[1] Cyclosporiasis is most common in tropical and subtropical regions of the world. In the United States, foodborne outbreaks of cyclosporiasis have been associated with several types of imported fresh produce (e.g., basil, raspberries, and snow peas). Validated molecular typing tools are not yet available, which could facilitate the detection and investigation of outbreaks C. cayetanensis.
Outbreaks of cyclosporiasis in humans have been reported mainly from North America, due to the sources of infection from contaminated fresh food products, such as soft fruits (raspberries), leafy vegetables (cilantro, basil and mixed salad) and herbs. Soil is another possible source of infection, especially in areas with poor sanitation.[2]
The Centers for Disease Control and Prevention (CDC) has been conducting national surveillance for cyclosporiasis since it became a nationally notifiable disease in January 1999. As of 2015, cyclosporiasis was a reportable condition in 42 states, the District of Columbia, and New York City. (NYC). Health departments voluntarily notify the CDC of cases of cyclosporiasis through the National Notifiable Diseases Surveillance System and submit additional case information using the CDC Cyclosporiasis Report Form or the Cyclosporiasis National Hypothesis Generating Questionnaire (CNHGQ).[3]
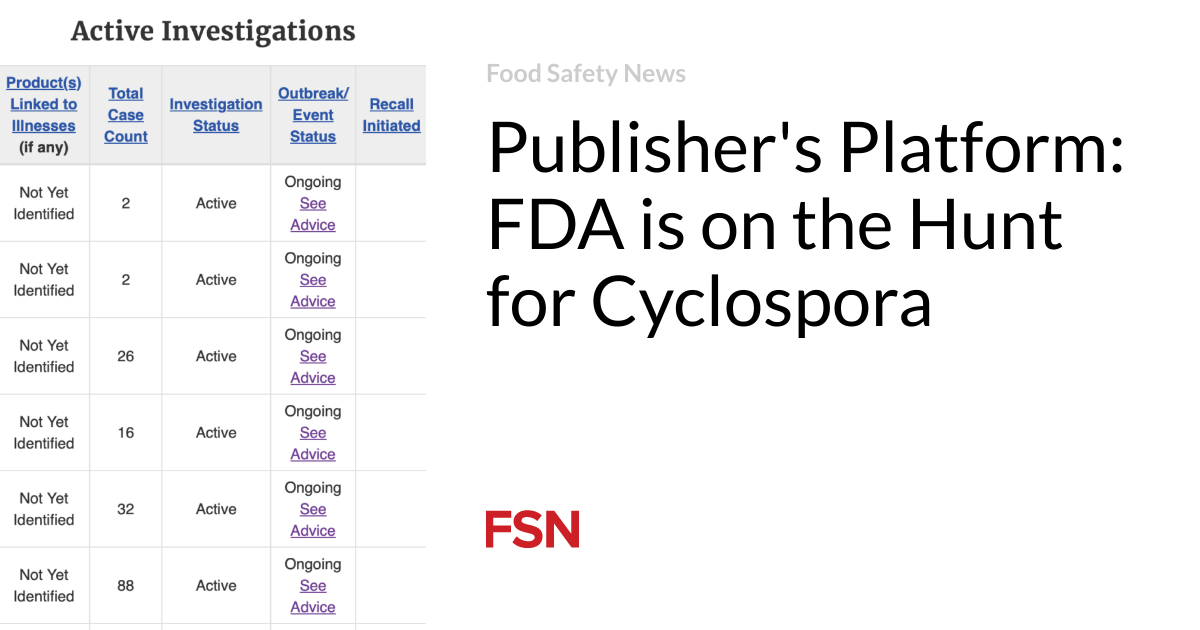
While cases of cyclosporiasis are reported year-round in the United States, cases of cyclosporiasis acquired in the United States (i.e., “domestically acquired” or cases of cyclosporiasis not associated with travel to a country classified as endemic is considered for Cyclospora) is most common during the spring and summer months. The exact timing and duration of U.S. cyclosporiasis seasons can vary, but reports typically increase beginning in May. Multiple outbreaks of cyclosporiasis were identified in 2020, linked to different products. As of September 23, 2020, the CDC documented 1,241 laboratory-confirmed cases of cyclosporiasis in people who had no history of international travel during the 14-day period before illness onset.[4]
What are the typical symptoms of Cyclospora infection?
Cyclospora infects the small intestine (intestine) and usually causes watery diarrhea, bloating, increased gas, stomach cramps and loss of appetite, nausea, low-grade fever and fatigue. In some cases, vomiting, explosive diarrhea, muscle pain and significant weight loss may occur. Some people who are infected with Cyclospora have no symptoms. The time between infection and becoming ill is usually about a week. If the disease is not treated, it can last from several days to six weeks. The symptoms may also return one or more times (relapse). In addition, people who have previously been infected with Cyclospora could become infected again.[5]

True Cyclospora come from?
The modes of transmission of C. cayetanensis are still not fully documented, although fecal-oral transmission is the main route. Direct transmission from person to person is unlikely. Indirect transmission can occur if an infected person contaminates the environment, the oocysts sporulate under the right conditions, and then contaminated food and water are ingested. The role of soil in transmission has also been proposed. The relative importance of these different modes of transmission and sources of infection is not known.[6]
The spread of infectious Cyclospora oocyst via water, soil and unprocessed foods (e.g. fruits and vegetables, including ready-to-eat salads) is made possible by their small size (8–10 μm), low specific gravity and high infectivity. Such oocysts can survive in water and food for weeks to months, depending on ambient temperature, and can withstand routine fumigation or chemical disinfection procedures used in irrigation systems, recreational water, or drinking water treatment plants.[7]

How are you? Cyclospora diagnosed?
Cyclosporiasis is usually diagnosed symptomatically in a clinical setting, including the presence of watery diarrhea, abdominal cramps, and bloating. In untreated, immunocompetent people, diarrhea may last for days to weeks to a month or more, and may wax and wane, with variable oocyst shedding. Oocysts may be shed (intermittently or continuously) by asymptomatic people, and symptoms may persist even when oocysts are not present in the stool. In a clinical context, conventional diagnosis usually involves microscopic examination of biopsy sections of intestinal tissue, stool samples for the presence of developmental stages of Cyclosporaor advanced molecular testing for DNA. Improved specificity and sensitivity have been largely possible through the use of PCR, which allows the specific amplification of genetic loci from small amounts of genomic DNA from Cyclospora. Due to the intermittent nature of oocyst shedding and the low numbers of this stage in the stool, it is recommended to collect multiple stool samples at 2 to 3 day intervals over a period of more than a week to increase the likelihood of identifying the oocysts. enlarge. disease microscopically.[8]
What are the serious and long-term risks of Cyclospora infection?
Cyclospora has been associated with a variety of chronic complications, such as malabsorption, reactive arthritis, and cholecystitis (inflammation of the gallbladder). Since Cyclospora infections usually respond well to appropriate treatment; Complications occur more often in people who are not treated or not treated quickly. Extraintestinal infections also appear to be more common in individuals with compromised immune systems.[9]
Although human cyclosporiasis is generally not fatal in developed countries such as the United States, prolonged diarrhea often leads to dehydration, especially in infants who are at greatest risk for severe dehydration and death, especially if cyclosporiasis is complicated by infections with other pathogens (viral , bacterial or parasitic, for example Cryptosporidium And Giardia), malnutrition or malabsorption, especially in disadvantaged communities.[10]
According to the CDC[11]the recommended treatment is a combination of two antibiotics, trimethoprim-sulfamethoxazole, also known as Bactrim, Septra or Cotrim. For people who have diarrhea, it is advisable to rest and drink enough fluids.
[1] Casillas, S. M., Hall, R. L., & Herwaldt, B. L. (2019). Cyclosporiasis Surveillance – United States, 2011-2015. Weekly Morbidity and Mortality Report. Surveillance Summaries (Washington, DC: 2002), 68(3), 1–16. https://doi.org/10.15585/mmwr.ss6803a1
[2] GiantasperoA., & Gasser, R.B. (2019). Human cyclosporiasis. The Lancet Infectious Diseases19(7), e226–e236. https://doi.org/10.1016/S1473-3099(18)30789-8
[3] Casillasi pray, Note 1 on page 1.
[4] CDC. (2020, September 24). Cyclosporiasis outbreak investigation – United States, 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/parasites/cyclosporiasis/outbreaks/2020/seasonal/index.html
[5] Cyclosporiasis – Disease. (2018, May 11). https://www.cdc.gov/parasites/cyclosporiasis/disease.html
[6] Almeria S, Cinar HN, Dubey JP. Cyclospora cayetanensis and Cyclosporiasis: an update. Microorganisms. 2019; 7(9):317.
[7] GiantasperoIdemNote 2 on page 1.
[8] GiantasperoIdemNote 2 on page 3-4.
[9] CDC. (2020, October 21). CDC – Cyclosporiasis – Resources for Healthcare Professionals. Centers for Disease Control and Prevention. https://www.cdc.gov/parasites/cyclosporiasis/health_professionals/index.html
[10] GiantasperoIdemNote 2 on page 2.
[11] CDC. (2020, September 17). CDC – Cyclosporiasis – General information – Frequently asked questions about cyclosporiasis. https://www.cdc.gov/parasites/cyclosporiasis/gen_info/faqs.html