Health
Why self-collected tests will change everything for cervical cancer screening
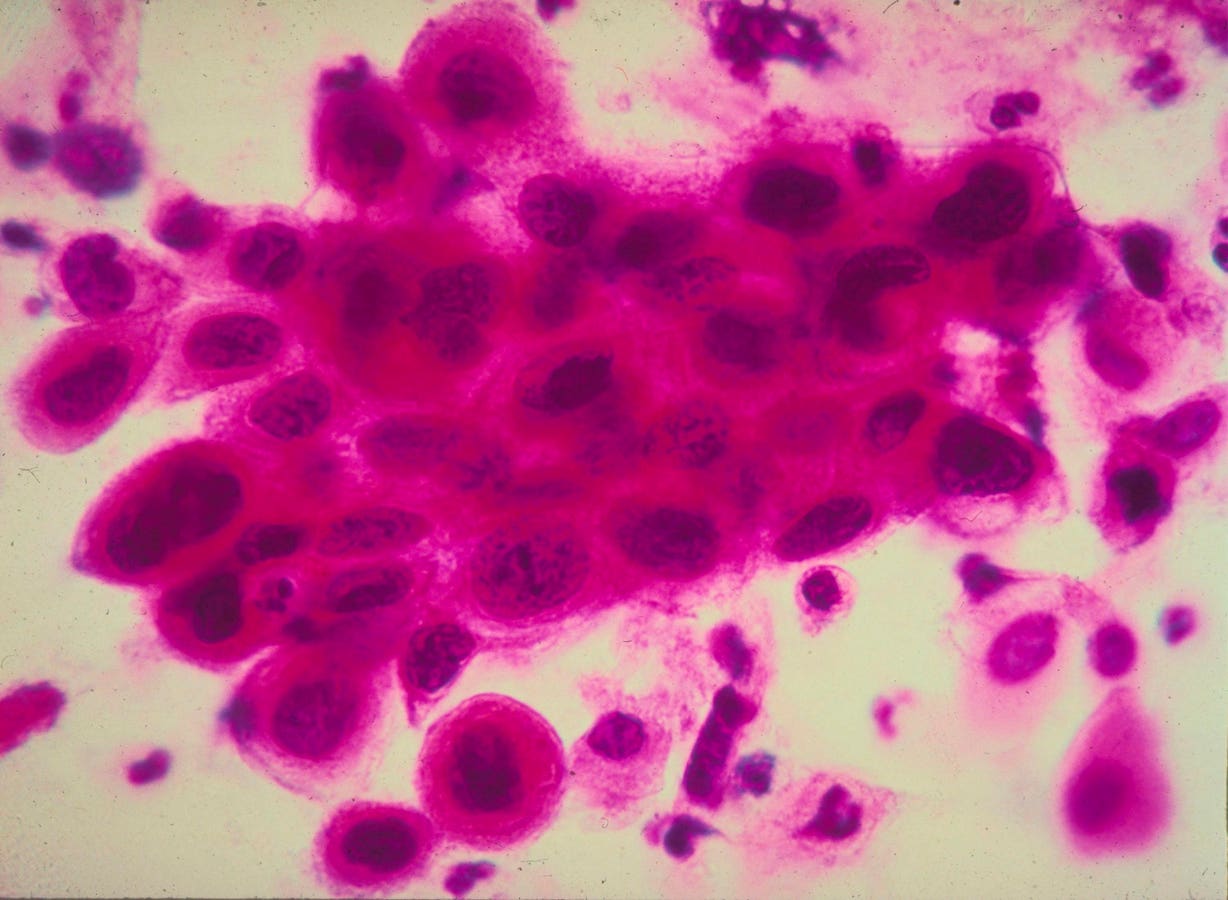
390487 02: (FILE PHOTO) Close-up of cancer cells in the cervix. Cancer of the cervix, the … [+]
In the autumn, women can test for cervical cancer with a simple, self-administered test. Self-sampling allows a woman to swab her vagina privately at a doctor’s office, after which doctors send the collected sample to a laboratory to test for cervical cancer. Home screening is currently under review by the FDA, but could be another option for women early next year, according to reports from The New York Times.
According to tradition, women are usually screened for cervical cancer with a Pap smear at age 21 CDC. In this test, a doctor inserts a speculum into the vagina with the patient’s legs apart while the doctor collects a small number of cells from the cervix.
For many women, a Pap smear is not the easiest or most comfortable test to obtain. In reality, research presents significant barriers associated with undergoing the test, including but not limited to the sheer discomfort and pain experienced from inserting a cold metal speculum into the vagina. Not only can the test be uncomfortable, but it can also cause significant cramping for hours after the short test is completed.
Women may also be reluctant to undergo the test out of embarrassment, privacy concerns about having to show a very private part of their body to a doctor. More than a third (38%) of women felt embarrassed about getting a Pap smear due to concerns about the smell of their vagina, according to a study reported by BBC.
Self-collected testing can remove many of these barriers because samples can be collected privately by a woman. Furthermore, a self-administered test only involves a simple swab of the vaginal area, similar to a Covid test swab that many are already familiar with. The cotton swab helps eliminate the incredible discomfort that many women experience during a Pap smear.
Self-examination, especially home screening, can significantly expand the reach of cervical cancer programs and reduce health disparities, especially in areas where health care resources are limited. Pap smears currently require an in-person visit to a healthcare provider. This geographic barrier can prevent people in low-income, underserved, or rural communities from getting the screening they need to save their lives. With at-home screening possibly starting early next year, women will no longer have to travel and can get screened from the comfort of their home. This would be the 23% of women who are currently unaware of their cervical cancer screening.
Finally, the ability to perform the screening test themselves can be empowering for women. Self-administration gives women control over their health, which can lead to better adherence to recommended screening guidelines. Having control over their own bodies has become an especially important topic of conversation given all the recent Supreme Court rulings on abortions in America. With self-collected screening, women will undoubtedly feel more comfortable and part of the care process.
This empowerment is especially critical in communities where discussing sexual health is taboo or in situations where women feel uncomfortable with a pelvic exam by a doctor. Self-collected testing can break down these cultural and social barriers while empowering women to take charge of their health.
Self-collected screening represents a significant step forward in addressing the barriers to cervical cancer screening. More than 11,000 new cases of cervical cancer are diagnosed in the United States each year, and estimates indicate that 4,000 women die from it. CDC. By making screening more accessible, earlier detection will lead to a reduced burden of cervical cancer in America.