Health
Dairy farmers are resisting the CDC’s insistence on PPE against the bird flu virus

WASHINGTON – The Centers for Disease Control and Prevention this week recommended that dairy and poultry farms with infected animals provide protective equipment to workers in an effort to prevent human transmission of the H5N1 virus. The challenge now is to make this happen.
The CDC has no legal authority to order these protective measures, and health officials in some of the nine states with reported outbreaks among livestock have had little luck getting farmers to take up offers of free personal protective equipment for their workers, even though the virus continues to spread. Six additional infected herds were reported yesterday – in Michigan, Idaho and Colorado – bringing the total to 42.
Texas, the only state with a confirmed human case involving a worker exposed to infected cows, has sent protective equipment to a number of farms – four to be exact. The state health department began offering gloves, masks, goggles and gowns to dairy farms in early April, shortly after the state’s first cases were identified. A handful of locations in the Texas Panhandle – each with sick cows – accepted them. The state has reported 12 infected herds so far.
“We offered PPE to every interested dairy and only four took up the offer. The offer still stands,” Texas Department of State Health Services Press Secretary Lara Anton told STAT in an email.
Similarly, in Idaho, the Department of Health began offering protective equipment to farms when federal officials did so confirmed the presence of the flu in a herd there early last month. They have had no takers. “We have not distributed any personal protective equipment to date,” said AJ McWhorther, a spokesman for the state health department.
In Michigan, which has now reported 10 herd infections, state officials have left coordination of personal protective equipment to local governments, meaning there is no realistic picture of protective measures on the ground. “We do not track PPE distribution from local health departments,” a health department spokesperson said.
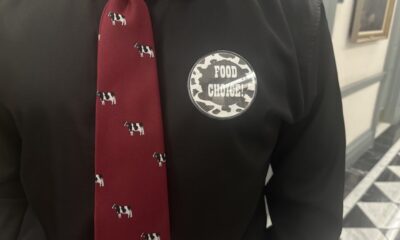
Dairy groups say their members fear financial ruin if their livestock is found to be infected, and lawmakers are also increasingly concerned that H5N1 measures could deter the industry. There is also the fact that protective equipment is not ideal for hot working conditions such as milking parlors. “These workers have foggy glasses all the time, which makes them more susceptible to injury,” said Michael Osterholm, an epidemiologist and director of the University of Minnesota’s Center for Infectious Disease Research and Policy. “N95 [masks] don’t necessarily work well if they get wet.
But while federal officials and infectious disease experts maintain that the risk to the general public is still very low, the threat is greater for those who come into contact with cows, especially since infected animals may not show outward signs of illness.
“The main risk at the moment lies with those who work in the actual milking processes. That’s a big question: what’s happening there? We don’t know,” Osterholm said.
It’s a big ask because the CDC and local health authorities rely on farmers’ cooperation to test not only cows, but workers as well.
Darren Turley, executive director of the Texas Association of Dairymen, characterized the human infection — a worker who developed pink eye — as a “one-off incident” involving an inexperienced temporary worker who may have gotten milk on his hand and then wiped his eye . .
“After that, we started offering face shields,” Turley said. “But the most important thing was to ensure that if you bring in an employee who is not used to working in areas with sick animals, he or she receives the appropriate training beforehand.”
While educating workers could minimize future transmission, there is no certainty as to how this happened in the first place. CDC and Texas officials are still can’t say whether the farm worker contracted the bird flu virus directly from a cow “because there are no specimens from cows or environmental factors samples were available …and epidemiological research could not be conducted on the farm.” They were also unable to collect samples from the workers and his roommates.
“It’s a combination where the local farms, as well as agriculture officials, have largely stymied public health efforts to get into those farms to conduct testing on individuals who work there,” Osterholm said.
That may be starting to change. Todd Davis, acting chief of the CDC’s Influenza Division’s Virology, Surveillance and Diagnostics Division, said at a World Health Organization event this week that the CDC is working with state and local health departments to initiate serology surveys testing the blood of farmworkers on evidence of past birds. flu infection.
Prioritizing masks and goggles for workers on farms with previously confirmed cow infections is a relatively modest step in understanding the scope of the outbreak, infectious disease experts said.
“That’s not enough,” Shira Doron, chief of infection control at Tufts Medicine and the hospital epidemiologist at Tufts Medical Center, said of the CDC’s recommendation to use personal protective equipment on farms with known H5N1 outbreaks. “It should be everything [dairy farms],” she said. “Once [cows] If they are ill, they will probably no longer be contagious within a few days, at which point they will be of least concern.
But the barrier for health officials is WHO would set off a push to largely mask and protect dairy farms, let alone potentially require safety measures. State and federal health agencies do not have that authority. Multiple state health departments told STAT that their staff have not set foot on farms with confirmed cases, citing “privacy and biosecurity reasons.”
The bureaucratic ties for human health agencies were clearly visible Monday in CDC Deputy Director Nirav Shah’s statement on the agency’s new recommendations. He asked state health officials to “work with their counterparts in the state Agriculture Department to identify farmworker organizations that can help coordinate and facilitate the distribution of PPE.” The recommendation ultimately lets the agricultural sector take the lead on protective measures – or bypass them.
“In an ideal world we would have a lot of oversight,” Doron says. “But in the real world we have farmers who may be operating on very narrow margins, who may already be in financial trouble, and have no structure to compensate them for doing the right thing, when the right thing could actually lead to a significant damage. financial impact.”
Megan Molteni and Helen Branswell contributed to this report.