Health
I am cautiously optimistic about the new treatments for Alzheimer’s disease

Group of people from different countries as sociological concept.
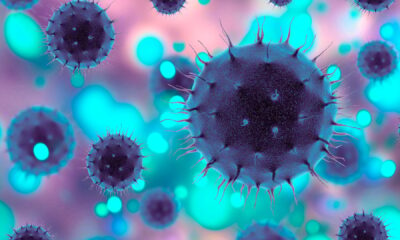
Alzheimer’s disease is a neurodegenerative disorder that manifests in the deterioration of brain functions such as memory, language, judgment and reasoning – to a point of complete immobility – making this condition a difficult diagnosis. From 2022 It is estimated that as many as 6.5 million people have dementia or dementia-related diseases. As Alzheimer’s and Brain Awareness Month comes to a close in June, we must also realize that with no cure in sight and limited accessibility of therapies that can slow progression, Alzheimer’s disease remains a tsunami headed straight for our healthcare system.
Researchers estimate the expected associated costs treatment and care for Alzheimer’s disease patients is expected to reach more than $1 trillion will affect almost 13 million people by 2050 – only in the United States. That bill is paid by Medicaid/Medicare, private insurers, out-of-pocket costs and other sources. Some people use their own money to supplement costs, but most of us can’t afford that.
Until the last few years, there was no viable therapeutic agent to minimize the progression of early Alzheimer’s disease. In 2023, the Food & Drug Administration fully approved it Leqembi (lecanemab), a promising new treatment shown to reduce the progression of early-stage Alzheimer’s disease. Donanemab, another drug that works to reduce symptoms of mild cognitive impairment, is expected to be fully approved in the coming months. Both drugs are undoubtedly an important advance in the fight against a devastating disease.
These medical breakthroughs have given me hope, but I worry about the looming health disparities they will cause. As a social epidemiologist with decades of research into social determinants of disease, I believe that the approval of Leqembi and Donanemab raises important ethical, safety and economic concerns that cannot be ignored by academia, healthcare and pharmaceutical stakeholders.
Two concerns in particular stand out:
No. 1: Lack of diversity in clinical trials.
Leqembi was evaluated based on a phase 3 clinical trial, which tested its efficacy and collected any side effects associated with the drug. The manufacturer’s clinical trial involved nearly 950 study participants, and of that total only 43 identified as black. Similarly, Donanemab had 1,182 study participants who were split into two randomized groups: 588 received the drug and 594 received a placebo. Only in each group 17 identified as black (3% of each group). Yet black populations have a two to four times higher risk of developing Alzheimer’s disease than non-Hispanic whites. Unfortunately, underrepresentation of many communities is common in most clinical trials involving minorities represent less than a tenth of clinical trial participants. Adequate representation of all communities in clinical trials is a matter of social justice and good science. Whether it’s a lack of culturally appropriate outreach efforts, eligibility criteria that disproportionately exclude Black and other minority populations, or participants’ distrust in our healthcare system, we need everyone to truly make some progress in our fight to end overcome Alzheimer’s disease. ™s disease.
No. 2: Economic burden on the majority of people.
A press release from Leqembi pharmaceutical manufacturers sets the price of the drug $26,500 per year where treatments are required indefinitely – completely out of reach for most Americans. This does not include the cost of the study, the administration of multiple treatment infusions in the clinic, and the required maintenance of brain scans. Fortunately, those with Medicare and supplemental insurance will pay much less, but those without insurance or insufficient insurance are left with an unaffordable option. This high price tag limits access to those who are financially disadvantaged and exacerbates existing healthcare inequalities. An additional barrier to consider: the allocation of healthcare resources to expensive treatments can also divert attention from preventive measures, early diagnosis and care for Alzheimer’s patients.
The approval of Leqembi, and others to follow, undeniably marks an important milestone in the fight against Alzheimer’s disease. However, it should be seen as a double-edged sword, involving both hope and fear. Alzheimer’s disease is a disease with many facets with different underlying factors, and although both Leqembi and Donanemab target the amyloid protein at different stages of build-up in the brain, we may be overlooking the complexity of its pathogenesis. Diverting resources away from other research directions, which could be equally promising and more inclusive for diverse participants, cannot and should not be overlooked.
Ethical considerations, long-term safety assessment and equal access to treatment must remain at the forefront of our medical community, regulators and researchers – guiding the responsible integration of Leqembi, Donanemab and hopefully future life-changing treatments. in the arsenal of tools to combat Alzheimer’s disease.