Health
The shortage of blood culture bottles will hurt patients in surprising ways
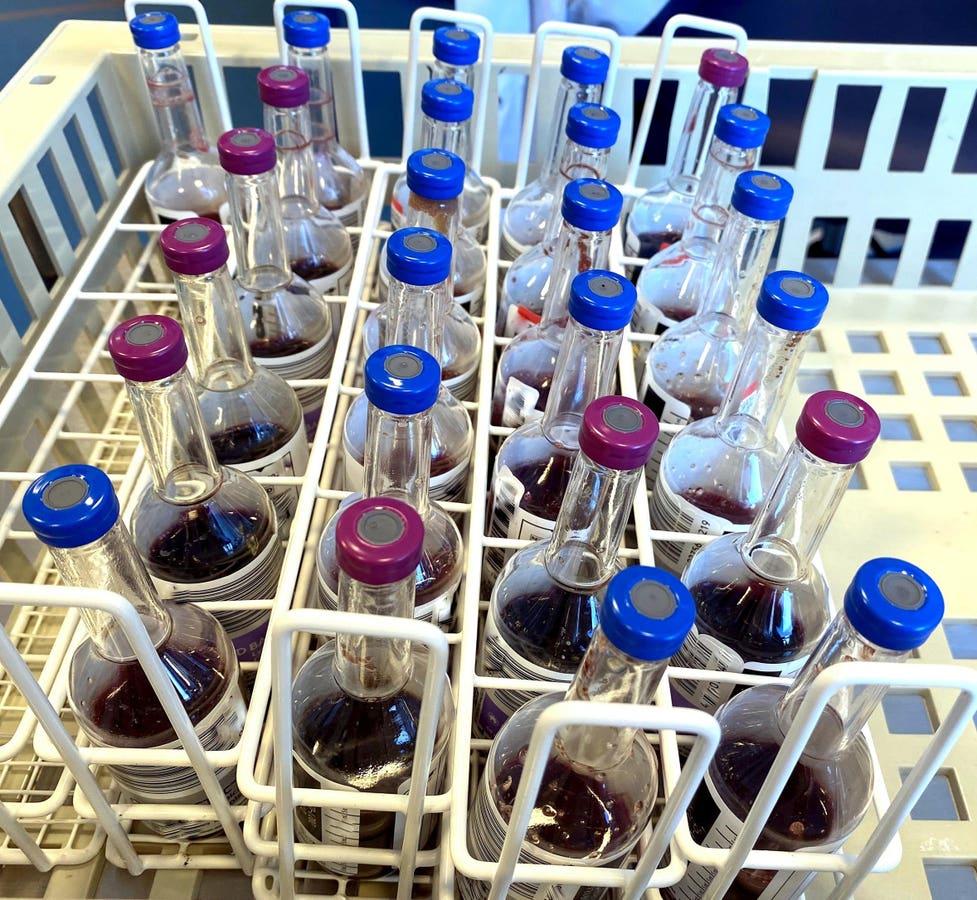
By culturing the blood, microbes can be identified and tested for resistance to antimicrobial drugs. … [+]
The Centers for Disease Control and Prevention has a Health Alert Network opinion on July 23 on a critical shortage of Becton Dickenson blood culture vials that will seriously disrupt patient care. They also kept one call doctor with the Infectious Diseases Society of America, the American Society of Microbiology, the Society of Healthcare Epidemiology of America and the Pediatric Infectious Diseases Society.
Although this sounds esoteric – why would anyone care about these bottles? – there is no doubt that this shortage will seriously harm patients. This is why.
When a patient comes to hospital with a severe infection or fever, one of the first things done is to take two sets of blood cultures to try to identify the source of the infection and identify the antibiotics that will most specifically target the infection. target the bacterial (or fungal) infection. ) perpetrator. Because blood is normally sterile, most of the bacteria growing in the blood culture are the source of the infection. Skin or fecal bacteria can sometimes cause an infection, especially on heart valves or foreign objects (such as a prosthetic joint). It can occasionally be difficult to determine whether the bacteria is a contaminant of the culture site that has not been properly sterilized or whether it is actually the pathogen. If this type of infection is suspected, two or even three sets of cultures are taken before starting antibiotics.
During this call from a doctor, Chris Beddard, vice president at BD Life Sciences, said the shortage could last until September. She alluded to a production problem with the source of the specially shaped plastic bottles used for the culture bottles, but did not go into details.
Dr. Romney Humphries, medical director of the microbiology laboratory at Vanderbilt University Medical Center, startled some attendees by pointing out how dire the situation was. They had learned of the shortage only a few days in advance. She said Vanderbilt “received a shipment of ten individual bottles for the entire 1,700-bed hospital.” Drawing just one set of cultures “is absolutely not the standard of care. But we have found ourselves in a situation where we cannot provide the standard of care for this shortage. So I think it becomes a risk decision. Is the lack of a blood culture for any patient worse or better than one set for all patients?”
Several speakers on the call suggested reducing the number of cultures performed by changing the criteria, such as not allowing repeat cultures within 48 hours. Others emphasized careful attention to sterile techniques to reduce the number of contaminants and the need for repeat cultures. Some suggested using expired bottles.
Please note that cultures from one manufacturer are not interchangeable with those from others due to the shape of the bottle or the type of machine they work with. Bactec is a leader in the US market. In terms of revenue, the value of the blood culture testing market was estimated $5.2 billion in 2023 and $7.6 billion in 2026. The top three companies in this niche are Becton Dickinson, Terumo and bioMérieux.
Participants raised several concerns, including the standard of care. Currently, sepsis guidelines (and quality assurance assessments) require that two sets of cultures be collected, usually within an hour of arriving at the emergency room, and before the patient is given antibiotics. Will doctors now be punished for pulling just one set?
One participant said he hoped the government would publicly note that this is a situation where crisis standards of care and rationing will kick in – both to inform the public and to reduce the chance of doctors being sued for malpractice for having only one set drawn.
Marsha Steed is a microbiology expert who has also had the misfortune of having repeated sepsis with an antibiotic-resistant individual E.coli. After the phone call, which she was also present at, she told me, “It was very, very scary,” and during a recent hospital stay, “they only took out one bottle, and it kind of popped out.” I know there are usually different bottles for different media that test for different types of bacteria. And they only use one bottle. And when the nurse did the draw, she didn’t say they were deficient, but she had said, ‘I have to be very careful when I take the sample because I can’t go under the volume and I can’t go through the volume , they want you to be very careful.’” During the conversation with the doctor, they also mentioned possibly using anaerobic or mycolytic (used for tuberculosis) bottles instead of the usual aerobic bottles. Steed responded, “You know, the aerobic types are really what’s probably going to give a better result and a wider range of organisms.”
Matthew Wynia, MD, MPH, is an infectious disease specialist and bioethicist. We discussed the recurring problem of relying on a single source for a product. I have long been concerned about a fragile supply chain and resulting shortages. A good example is the shortage of the basic product IV saline, which occurred after production at the Baxter plant in Puerto Rico was halted due to hurricanes. They produced 43% of the US market’s IV saline needs.
Wynia noted, “Dozens of reports have been written on how to address drug shortages, and they all recommend that we shouldn’t have a sole source for anything. You need diversification of your supply chain.” He added that “just-in-time delivery of the cheapest possible product” contributes to the problem, just as this is “the equivalent of a generic drug.”
Wynia has long been concerned about moral problems caused by coercive actions. He said: “We may never fully recover psychologically from the pandemic and the moral distress that comes with having patients who needed something, and we couldn’t give it to them because we didn’t have it.” He sees the same thing happening now with this critical shortage of blood culture bottles. He also wondered what patients would hear.
A final concern I have raised is the use of unnecessary broad spectrum antibiotics to ‘cover’ potentially resistant organisms. This will predictably lead to superinfections with more resistant organisms, fungi or C. difficult diarrhea. This was seen, for example, when a deficiency of piperacillin-tazobactam led to increased use of meropenem and subsequent C. difference.
But the bottom line is that this shortage of blood culture bottles will result in difficult decisions about triage and rationing, and both doctors and patients will be hurt, albeit in different ways.













